In-Vitro Fertilization And Embryo Transfer (IVF)
In-vitro Fertilization and Embryo Transfer (IVF)
In-vitro fertilization and embryo transfer (IVF) is an effective method to help couples who are unable to conceive naturally. Broadly speaking, it involves the following steps: ovarian stimulation— medication is used to boost the ovaries to produce more eggs; egg collection— a needle is inserted into the ovaries via the vagina to collect the eggs; sperm processing and fertilization— the eggs are mixed with the sperms in the laboratory; embryo transfer— to return the embryos into the womb.
IVF is used to treat:
![]() Men with poor semen quality;
Men with poor semen quality;
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Ovarian stimulation
The treatment cycle starts on the 2nd or 3rd day of your period. An internal (vaginal) scan will be performed at this visit to make sure that you do not have cyst in the ovaries. Blood may be taken to check hormone levels especially if this is the first treatment cycle.
If all are well, you will be given hormone injections to stimulate your ovaries so that multiple follicles (each containing an egg) will develop. You will be taught how to give the injections by yourself, or you can arrange injections to be done at the clinic. The hormone injections are to be done every day for around 8 to 10 days, depending on how fast the follicles grow. During this period, you will be asked to attend the clinic 2 to 4 times to check the growth of the follicles by ultrasound scans. Blood may be taken to check hormone levels if necessary. Another injection drug, known as an antagonist, will be added in the latter part of the stimulation period to prevent your body from releasing the developing eggs too soon. When the largest follicle is ≥ 18 mm in size, it implies that the egg(s) is/are ready, and you will be asked to give an ovulation trigger injection to help the eggs mature. Blood will usually be taken to check hormone levels on this day.
This protocol is the most suitable one for the majority. However, some patients may need adjustments according to their individual condition. Your doctor will help you decide on the most appropriate protocol.
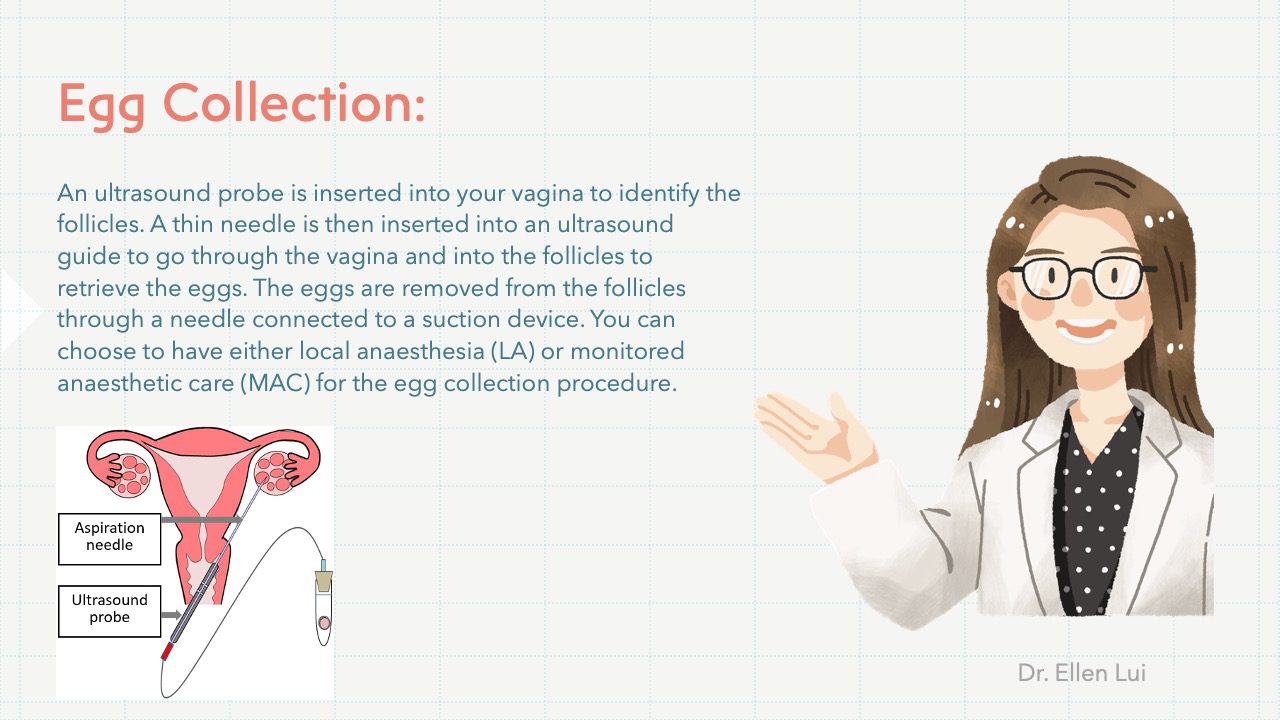
Egg collection
The eggs will be collected from your ovaries about 34–36 hours after the ovulation trigger injection. This is performed in Hong Kong Assisted Reproduction Centre (an IVF centre) with the help of an ultrasound scanner. An ultrasound probe is inserted into your vagina to identify the follicles. A thin needle is then inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs. The eggs are removed from the follicles through a needle connected to a suction device.
You can choose to have either local anaesthesia (LA) or monitored anaesthetic care (MAC) for the egg collection procedure. If you choose to have LA, you will be awake during the entire procedure. A local anaesthetic drug will be injected inside the vagina to reduce the pain level during the egg collection. Alternatively, MAC can be given by an anaesthetist who will be giving you anaesthetic drugs via a drip placed at the back of your hand, and you will be sleeping through. You can learn more about anaesthesia by referring to the information sheet on Anaesthesia.
The whole procedure will usually take around 30-45 minutes. After the egg collection, you should rest in the IVF centre, and your condition including blood pressure and pulse will be monitored. If everything goes well, you can go home 2 hours after the procedure, accompanied by an adult. You will need a day off on the day of the egg collection, but can return to work the next day.
Sperm processing and fertilization
The husband will be asked to produce a semen sample on the day of the egg collection. He can produce the sample at home or at the IVF Centre, whichever way he prefers. Freezing of a semen sample should be arranged in advance if he has problems in producing a sample on that day.
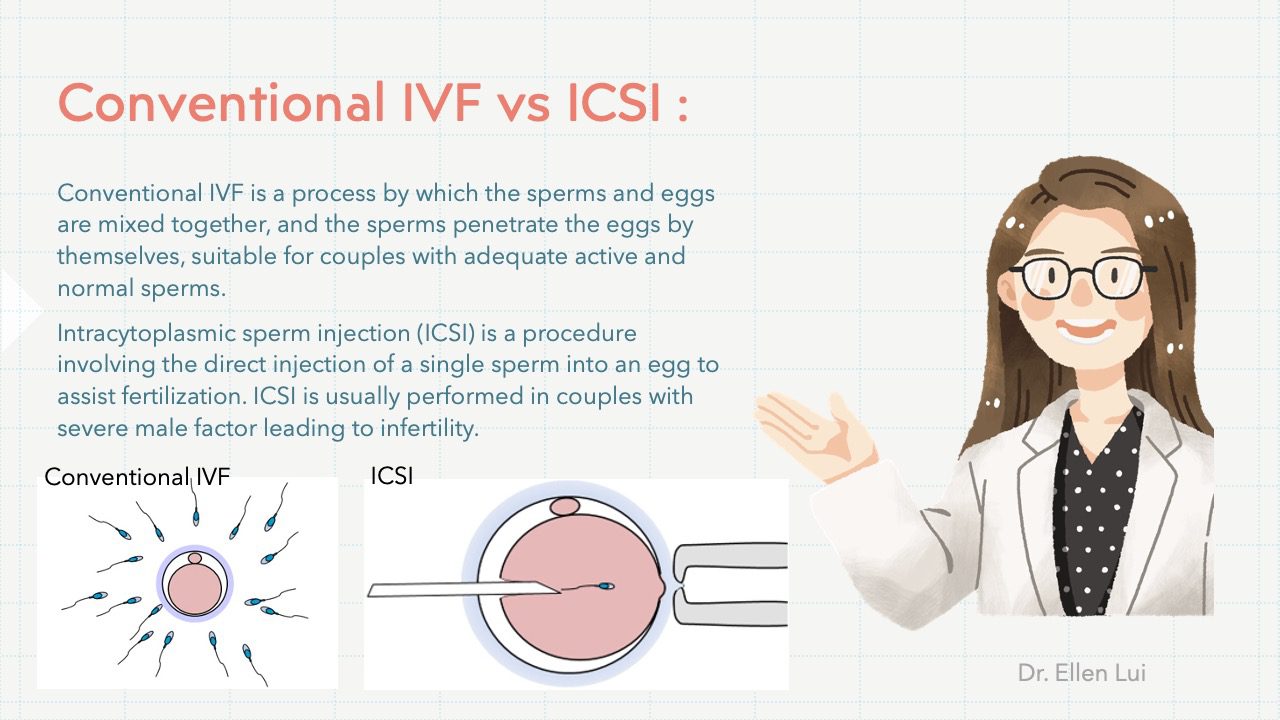
The semen sample will be processed, and the sperms will be used for insemination with either Conventional IVF or Intracytoplasmic sperm injection (ICSI).
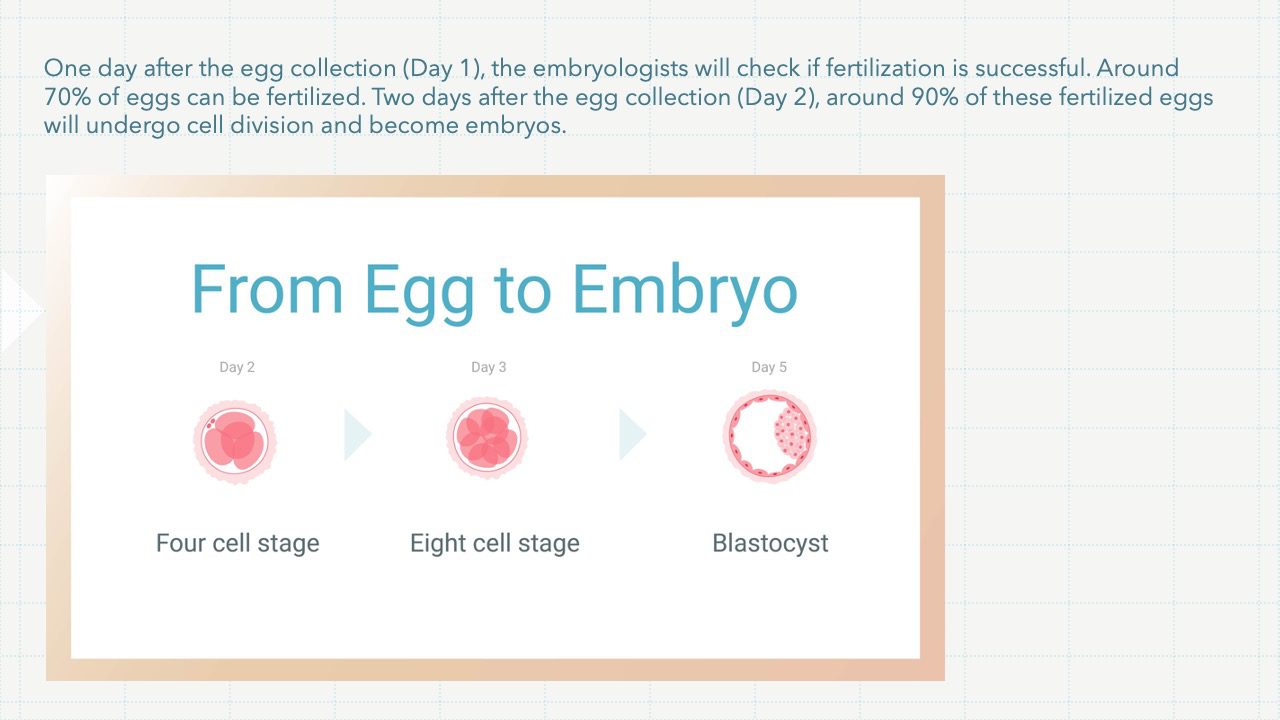
One day after the egg collection (Day 1), the embryologists will check if fertilization is successful. Around 70% of eggs can be fertilized. Two days after the egg collection (Day 2), around 90% of these fertilized eggs will undergo cell division and become embryos.
Embryo transfer
While the embryos are growing in the laboratory, you will need progesterone, and may be estrogen as well, to prepare the lining of the womb for embryo transfer. These are usually taken as pessaries which you can insert into the vagina yourself. The embryos will be ready to be returned to your womb 2 to 5 days after the egg collection (Day 2, Day 3 or Day 5). A small tube (catheter) is inserted through the cervix (the neck of the womb) and the embryo(s) is/are put into the womb cavity. Anaesthesia or analgesia is usually not required for this procedure. You can return to work on the same day or the next day. Your doctor may arrange a blood test a few days later to check your hormone levels to help decide if you need extra medications. You will be given a date to do a blood test for pregnancy, usually around 2 weeks after the egg collection.
Because of the risk of having a multiple pregnancy, only 1 or 2 embryo(s) will be put back into the womb. Under special situations, a maximum of 3 embryos can be replaced. Any remaining embryos that are of good quality will be frozen for use in the future, in case treatment does not work or to try for a sibling. They can be stored for up to a maximum of 10 years. Women in certain circumstances can store their embryos for up to 10 years or when they are 55 years old, whichever is later.
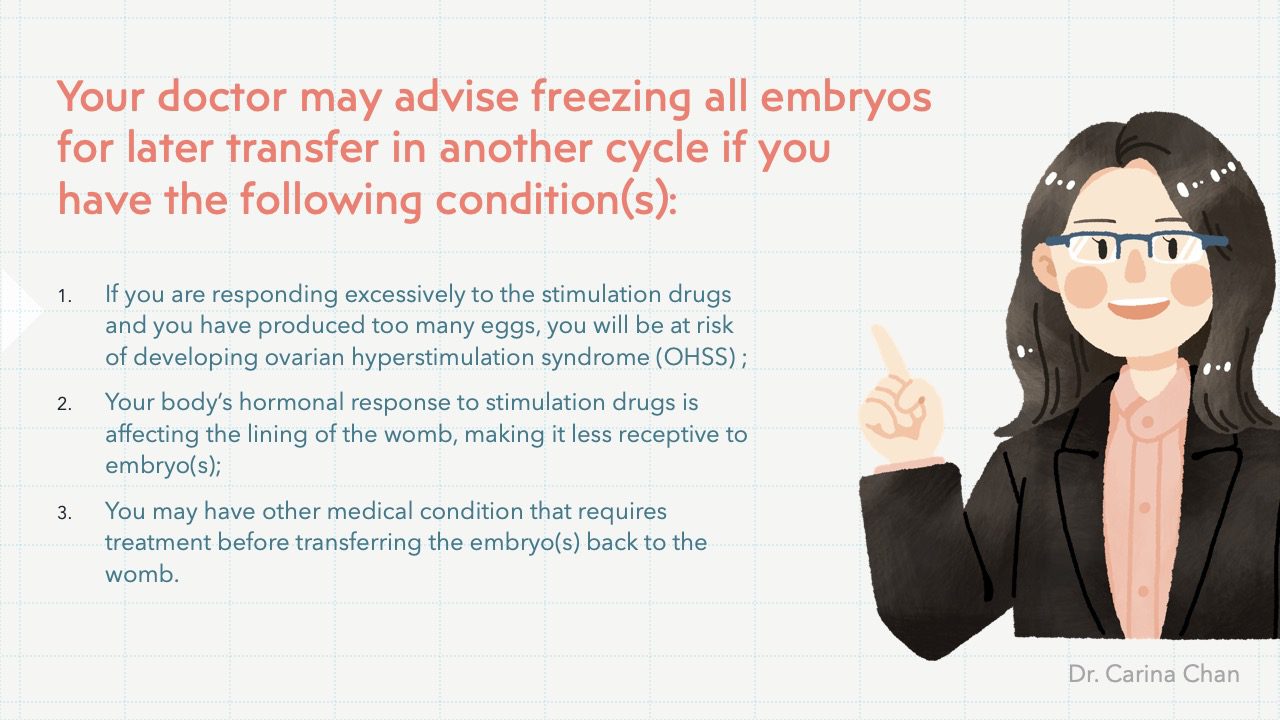
In a normal IVF cycle, the embryos can be returned to your womb a few days after the egg collection in the same cycle and any remaining suitable embryos are frozen. Your doctor may advise freezing all embryos for later transfer in another cycle if you have the following condition(s):
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Success rate of IVF
The pregnancy rate of IVF treatment is around 30-40% per cycle in general. As with all fertility treatments, the success rate of IVF depends on many factors such as the woman’s age, the cause of infertility, any history of previous pregnancy, response of the ovaries to stimulation etc.
Safety of IVF
IVF treatment is generally very safe. Most women are no more likely to experience problems with their health or pregnancy than women who have conceived naturally. However, there are some risks to be aware of, which range from mild discomfort to more serious conditions.
A multiple pregnancy (twin, triplet or more babies) can seriously harm the health of both mother and babies. At least half of twins are born premature and underweight, which can lead to serious health problems. Mothers of multiple pregnancies are also more likely to suffer from health problems such as high blood pressure, diabetes, and excessive bleeding during and after delivery than mothers of single babies. Selective fetal reduction in early pregnancy can be considered when a woman is carrying 3 or more fetuses. The procedure, however, is not without risk and may result in miscarriage and loss of all fetuses.
An ectopic pregnancy is when a pregnancy develops outside of the womb, usually in the fallopian tube. Ectopic pregnancy can happen with IVF (~5%) because the embryo(s) after transferred to the womb, can travel to the fallopian tube by itself/themselves. In rare occasions (<1%), heterotopic pregnancies can happen. This is when two pregnancies develop together, one in the womb and the other in the fallopian tube.
Ovarian hyperstimulation syndrome (OHSS) refers to an excessive response after ovulation stimulation drugs, resulting in too many eggs developing in the ovaries, which become very large and painful. Symptoms of OHSS include swollen stomach and stomach pain, nausea and vomiting, shortness of breath and reduced urine output. These symptoms usually appear a few days after the ovulation trigger injection and resolve when period returns. Mild OHSS is common and usually does not require any treatment. Very few women will develop severe OHSS (< 1%). In very rare cases, severe OHSS can be life-threatening.
Ovarian torsion is a condition that occurs when an enlarged ovary twists around the ligaments that hold it in place. This twisting can cut off blood flow to the ovary. If the blood restriction continues for too long, it can lead to tissue death and the ovary may have to be removed. This is a rare event with ovarian stimulation (<1%).
Use of an aspiration needle to collect eggs could possibly cause pelvic infection, bleeding, or damage to the bowel, bladder or a blood vessel. These damages are rare because the process is done under guidance with an ultrasound scanner. Risks are also associated with anaesthesia.
Although some early studies suggested a possible link between certain medications used to stimulate egg growth and the development of a specific type of ovarian cancer, more recent studies do not support these findings. There does not appear to be a significantly increased risk of breast, endometrial or cervical cancer after IVF.
Some previous research has suggested that fertility treatment may be associated with an increased chance of birth defects. Latest research believes that the birth defects are a result of fertility problems in the couples, rather than the fertility treatment itself. The incidence of birth defects in the general population is around 3%. In couples with infertility who subsequently conceive naturally, the chance of them having a baby with birth defect is slightly higher (~4%), which is the same as that in babies conceived through IVF. ICSI may carry slightly more risk.
![]()
![]()
Psychosocial support
Fertility treatment can be an emotional rollercoaster. So getting support from people who can relate to what you are going through is very important. Your spouse and your doctor can be a wonderful source of comfort and for some people that is enough. However, some people find it helpful to get extra support from a counsellor or a psychologist.
Recommended Video
![]()
![]()
Recommended Infographics
Any questions About Our Clinic?
Don't Hesitate to Contact Us
Contact number
(852) 2117 3033
gratia@hk-gmc.com
Opening Hours
MON - FRI :
0900-1800
(Lunch hour 1400-1500)
SAT :
0930-1330
Closed on Sundays & Public Holidays